Internal Medicine Medical Billing
Remote billing experts dedicated to improving collections & lowering overhead for internal medicine practices. Whether you are a solo internist or a multi-provider internal medicine clinic, our internal medicine medical billing services are designed to increase cash flow, reduce administrative burden, and streamline your operations.
Internal Medicine Medical Billing Is Not New To Us
Internal medicine billing is complex, time-sensitive, and frequently misunderstood by generic billing companies. Errors pile up, denials increase, AR ages rapidly, and practices lose money without realizing it. Providers become overwhelmed, forced to spend time on paperwork instead of patient care.
Mediclaim Pro Billing solves this with specialty-trained billers, accurate coding, proactive denial prevention, and seamless EHR integration. We give you the financial stability and administrative support needed to run a successful internal medicine practice.

Why Internal Medicine Practices Choose Mediclaim Pro Billing
- Specialized billing for internal medicine with certified coders trained in E/M, transitional care, preventive visits, and multi-diagnosis coding.
- Remote billing solutions that significantly reduce in-house overhead and eliminate staffing challenges.
- Specialists trained for every internal medicine EHR, including Athena, Kareo, ECW, NextGen, DrChrono, CareCloud, and more.
- Dedicated account manager providing weekly updates and direct communication.
Our Services
Internal Medicine Medical Billing Services We Provide
End-to-End Billing
We manage the full revenue cycle, charge capture, claim submission , payment posting, patient statements, and follow-up, with a workflow designed specifically for internal medicine practices. This ensures cleaner claims, higher accuracy, and faster reimbursements.
Coding & Audits
Our certified coders are experts in internal medicine guidelines, E/M levels, and chronic care coding. We regularly audit documentation, correct coding gaps, and optimize E/M levels to protect your practice from underbilling and compliance risks.
CCM & Preventive Services Billing
Internal medicine practices rely heavily on CCM, TCM, AWVs, and preventive services. We ensure correct documentation, frequency compliance, and coding accuracy so your practice captures every eligible dollar.
Electronic claim submission
Our billing pros accelerate your reimbursements by closely monitoring the adjudication timelines and claim submission statuses. We ensure to submit clean claims electronically to payers and timely follow up on any outstanding claims.
Denial management
Denials cost you money. MediClaim Pro Billing has a dedicated team for tracking your denials. We track the root cause of rejections or denials and execute targeted appeals with supporting documentation to recover revenue.
Insurance Verification
Insurance errors are one of the top causes of denials. We perform proactive eligibility checks, prior authorizations , and benefit verifications to prevent payment delays and reduce patient billing issues.
Denial Management
We aggressively resolve denied or underpaid claims by identifying the root cause, fixing systemic errors, and filing detailed appeals. Our strategies significantly improve recovery rates and reduce future denials.
AR Management
We track every dollar, reduce aging claims, and clean up backlogs. Our AR team ensures accurate payment posting and consistent follow-up, helping internal medicine practices maintain steady, predictable cash flow.
Payer Enrollment
We manage the complete credentialing lifecycle, including new enrollments, CAQH updates, revalidations, and payer negotiations. Our team ensures your providers remain active with insurance companies to avoid reimbursement interruptions.
EHR Integration
Our billing team integrates seamlessly with your internal medicine EHR and practice management system. We streamline workflows, reduce claim rejections, and eliminate manual data errors caused by system mismatch.
Performance Insights
We provide transparent monthly financial reports, denial trend analysis, CPT performance insights, and specialty KPIs. These reports help you understand revenue health, identify gaps, and make data-driven decisions.
Internal Medicine EHR Integration & Support
Our team works inside your internal medicine EHR, adapting to your current workflows so your staff does not need to change systems.
Find Your EHR/EMR








Security, Compliance & Reliability
Your billing partner must be secure, stable, and compliant. We safeguard your practice against industry-wide outages, billing delays, and data risks. Mediclaim Pro Billing ensures:
- HIPAA-compliant workflows
- Encrypted data handling
- Secure remote access
- Audit-ready documentation
- Redundant claim submission pathways
- Business continuity plans to avoid disruptions

How Our Process Works
We evaluate your current billing performance, identify leaks, and create a customized plan.
Our team follows up daily on all pending claims, denials, rejections, and appeals—until payment is secured.
We scrub all claims for accuracy, compliance, and payer-specific requirements before submission.
You receive monthly reports, weekly updates, and full visibility into your collections.
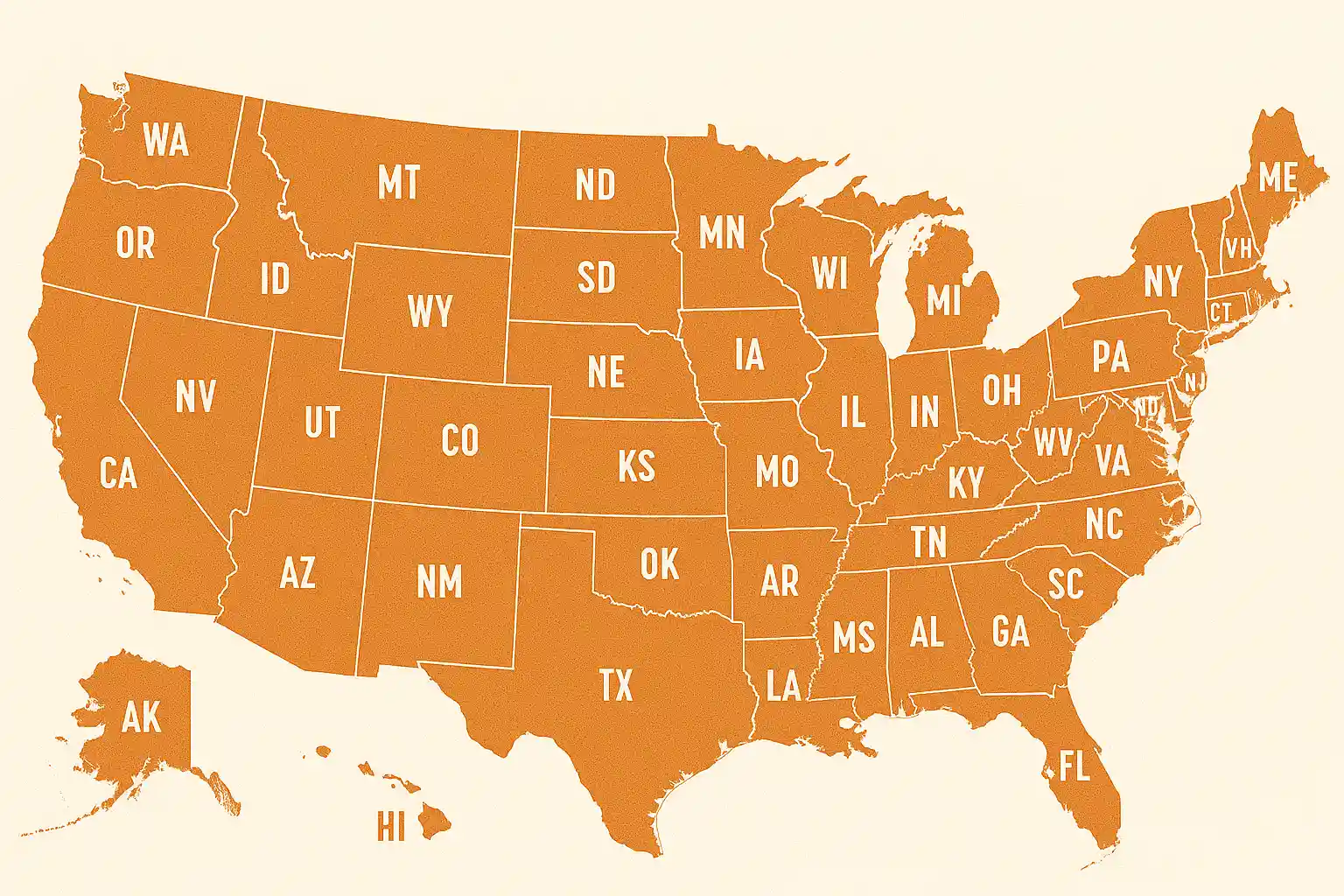
Internal Medicine Medical Billing For Every State
Mediclaim Pro Billing supports internal medicine practices across all 50 U.S. states. Whether you’re a solo internist or a multi-location group, our remote billing services connect seamlessly with your systems, allowing us to provide fast, compliant, and accurate support nationwide.
Simple Onboarding in 3 Steps
Schedule A Free Call
Schedule a free consultation with our mental health billing services specialist to share your ongoing billing challenges.
Free Revenue Audit
Our experts will review the 30 days of revenue and claims data to identify bottlenecks and revenue leaks.
Get Onboarded
Sign the BAAs and service agreement to officially begin the partnership. Our team will take over the charge asap.
Your Time Belongs With Your Patients, Let Us Handle The Billing

Frequently Asked Questions
Specialized billing is crucial for internal medicine because the specialty deals with high patient volume, diverse diagnoses, and complex treatment plans that require precise coding. Generic billing teams often miss nuances like chronic condition management codes, transitional care management, prolonged visits, or bundled services, which can lead to underbilling or claim denials.
Not at all. In fact, most clients feel they gain more control because of the transparency and reporting we provide.
Onboarding typically takes 3–7 business days, depending on your EHR setup and credentialing status.
Yes, we work seamlessly with all major internal medicine EHR systems. Whether your practice uses Athenahealth, Epic, NextGen, eClinicalWorks, Kareo, AdvancedMD, or another platform, our team integrates directly into your existing workflow.
The cost of internal medicine billing services typically depends on your practice size, patient volume, and the complexity of your billing needs. Most practices prefer a percentage-based model, usually between 4% and 8% of monthly collections. This ensures that you only pay based on the revenue we successfully collect on your behalf.
Specialty knowledge, transparent pricing, remote cost savings, and measurable results.
Absolutely. Most internal medicine practices serve a high percentage of Medicare patients, and our billing workflows are built around Medicare’s specific rules.
