Common Medical Billing Mistakes That Most Doctors Make
- Author : Mark Twain
- Date : 21/09/2025
Every doctor wants to gain their patients’ trust. However, a few common medical billing mistakes can damage that trust quickly. Billing mistakes create confusion with financial stress and frustration for both doctors and patients. The good news is that most billing problems can be avoided with better awareness and strategies.
What are those common medical billing mistakes that doctors should focus on? These errors usually involve coding, documentation, and communication failures. By understanding the root causes, doctors can take practical steps to prevent repeat problems.
In this blog, we will explore mistakes, their impact, and real strategies for correction. You will also learn about professional billing companies such as MediClaim Pro Billing and their impact. Let’s begin by identifying the biggest challenges in billing and coding.
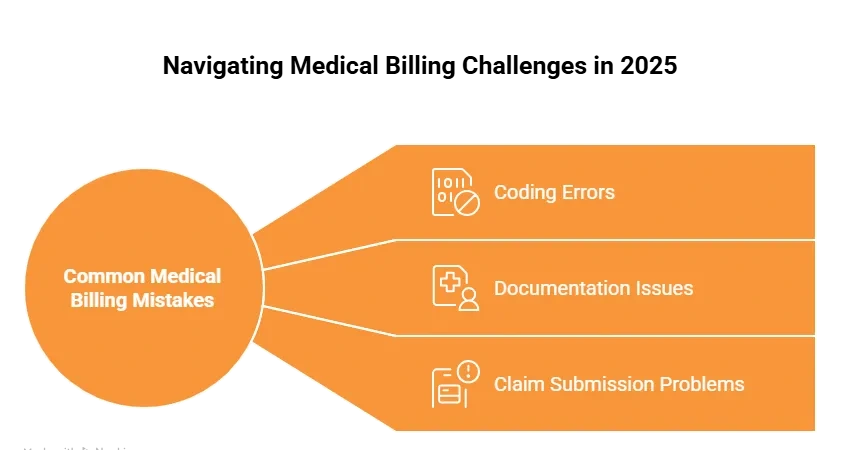
The Most Common Medical Billing Mistakes
1. Incorrect Patient Information
Even small errors in patient details can create big problems in billing. Spelling mistakes in a name or in an address can cause claim denials. Wrong date of birth entry or a single wrong digit entry in insurance numbers often leads to rejections and long payment delays.
Patient demographics, if entered without careful review, can cause claims to get stuck in the system and cause unnecessary delays and extra administrative work to fix the errors. Missing or mismatched insurance details like such as policy numbers or provider information, can trigger serious repeated claim rejections, leading to frustration.
2. Inaccurate Coding
Medical coding errors are the most common medical billing mistakes seen in clinics and hospitals. A single wrong diagnosis code entry or procedure code entry can cause rejected claims, payment loss, and even compliance risks.
CPT, HCPCS, and ICD-10 outdated understanding of coding guidelines often results in repeated errors and denied claims. Absence of proper coding review can even increase the chances of billing inaccuracies and compliance issues.
3. Missing Documentation
The lack of documentation is another major reason for claim denials. A medical record must include full details such as patient history along with treatment notes, test results, and follow-up care. Unclear or incomplete files often cause insurance rejection and delay claims.
Missing documents can create disputes between doctors as well as patients, and insurance providers. Also, delayed or inconsistent file updates lead to errors and repeated claim denials.
Pro Tip: Implement a checklist system for patient records. It prevents small mistakes from creating larger financial problems later.
Impact of Medical Billing Errors on Your Practice
Revenue Loss
Medical billing errors create serious challenges for doctors and healthcare practices. The most direct impact is revenue loss. Cash flow is lowered by denied or postponed claims, and fixing them takes more time and money. These errors can eventually result in large financial losses that compromise a practice’s feasibility.
Patient Trust Issues
Another major concern is patient trust. Patients start to question the systems fairness when they encounter billing mistakes like inaccurate charges or hold-ups in insurance claims. Some patients may decide to switch providers as a result of ongoing problems that stress them out. On the other hand, clear and accurate billing promotes lasting, solid patient relationships.
Compliance Risks
Errors in medical billing can cause doctors to have major compliance issues. Incorrect coding or insufficient documentation might give rise to government or insurance audits. Government or insurance audits may result from improper coding or a lack of documentation. Errors that happen again increase the risk of stricter oversight and reputational damage to a doctor.
How to Correct Medical Billing Errors in Healthcare
Step 1: Find the Error
- The first step is to verify the kind of billing mistake.
- Whether it is demographic, coding, or documentation-related, identification is key.
- Without knowing the error, correction becomes impossible.
Step 2: Contact the Insurance Company
- Once identified, notify the payer about the mistake.
- Submit corrections within the required time period to avoid rejections.
- Quick action is important to maintain a smooth cash flow.
Step 3: Train Your Staff
- Training is important for avoiding making similar mistakes repeatedly.
- Every staff member should understand how to correct medical billing mistakes.
- Investing in staff training pays off through fewer denials.
How Medical Billing Service Providers Can Help You
Medical billing services help doctors in taking care of claim submissions as well as coding, and follow-ups. This reduces the stress of their paperwork, so doctors can focus more on treating patients instead of handling billing tasks.
These services also improve efficiency because billing experts are trained to find common errors early. Billing professionals ensure higher claim acceptance and fewer denials with the use of advanced technology and audit systems. Outsourcing billing reduces overhead costs for clinics while increasing financial stability.
Companies like Mediclaim Pro Billing offer customized solutions to doctors’ problems that promise correctness as well as compliance, and faster reimbursements, so as to improve practice revenue.
Pro Tip: If your clinic gets denied a lot, it may be cheaper to outsource billing than to hire more staff.
Strategies To Avoid Mistakes in Your Medical Billing
1. Improve Data Verification
One of the main causes of claim denials is inaccurate or lacking patient information. Clinics must implement an organised data verification procedure to avoid this.
- Whenever patients sign up or book appointments, always double-check their insurance details and personal info because even small mistakes in insurance numbers like birthdays, or even name spellings can lead to rejected claims.
- Check entries again one more time before sending for claims to make sure they are correct and free from all errors. Most mistakes can be found by using a computer program or having someone else look it over again.
- Updating patient records and always asking for ID cards and insurance information when a patient comes in can help make sure that the data is correct.
- Getting the data right not only stops claims from being rejected but also saves staff time and makes patients trust you more.
2. Regular Coding Training
Medical coding rules can change frequently, so even small errors can bring compliance issues and revenue loss. Keeping staff trained is necessary.
- Ensure that coders and billers receive consistent training on ICD-10, CPT as well as HCPCS codes to ensure that they are informed of the most recent regulations.
- If people talk about their mistakes in the right way at regular team meetings, they can get better at writing code.
- Encourage certification or refresher courses for coding staff. Certified coders are better equipped to handle complex cases and reduce errors.
- Well-trained team not only ensures compliance but also reduces the chances of repeated claim rejections.
3. Technology Integration
Modern technology plays a big role in reducing billing mistakes and streamlining the process.
- Electronic Health Record systems are integrated with billing software to minimize manual errors. Use of integration ensures that patient data as well as documentation, and billing are connected seamlessly.
- Leverage automation and AI-driven tools to check for missing along ith duplicated, or even incorrect information before submission. Smart alerts can prevent errors at the source.
- Adopt claim-scrubbing software that reviews claims for accuracy against payer-specific rules before submission. This step can significantly cut down on denials.
- Dashboards usage and reports to track denial patterns and help in identifying weak areas, and improve future billing cycles.
Most Common Medical Billing Errors and Their Solutions
Demographic Mistakes
- One of the most frequent errors in medical billing comes from incorrect patient details. Any mistake in spelling, date of birth, or insurance number can lead to a claim being turned down.
Solution: Always verify patient information during every visit. Using digital forms and electronic systems helps reduce handwriting-related mistakes and ensures greater accuracy.
Duplicate Billing
- Submitting the same claim twice is another common problem. This often happens when multiple staff members handle billing without a proper tracking system.
Solution: Track claims through an organized system and assign clear responsibilities. Double-check before entering charges to avoid duplication.
Upcoding and Under-coding
- Coding errors can either overstate or understate the services provided. Both of these situations pose risks to compliance and could cause a loss of revenue.
Solution: Make sure that the documentation shows exactly what services were provided. Internal audits must be done on a regular basis to find and fix wrong coding before claims are sent in.
Failure to Track Claim Status
- Many claims remain unpaid simply because doctors and their staff forget to track them. Revenue delays can be avoided by keeping an eye on claim progress.
Solution: Use software that tracks claims in real time and sends alerts for claims that are still being processed or have been denied. This ensures no payment opportunity is missed.
Mismanagement of Denials
- Some practices ignore denied claims, considering them a loss. However, timely appeals can successfully recover revenue.
Strategy: Set up a separate process for managing denials and teach your staff to quickly look over the reasons for denials, fix any mistakes, and resubmit claims.
Outdated Billing Processes
- Using old software or systems that have to be set up by hand leads to more mistakes and slower work. Old ways of doing things also do not work with the new compliance rules.
Solution: Upgrade to modern billing systems with built-in coding updates such as error checks and reporting tools. This improves efficiency that ensures compliance, and helps maximize reimbursements while reducing administrative stress.
Conclusion
Medical billing mistakes can cause doctors to lose money and make patients disappointed, which could even get them in trouble with the law. The good news is that these mistakes can be fixed by training staff along with doing regular checks and making billing systems better.
With experts like Mediclaim Pro Billing, the process can be simplified and made more precise. You just sign the BAA, and then let them handle all your billing processes. Such companies have professional billers with years of experience and only charge a small percentage of your total collections.
Frequently Asked Questions
Coding mistakes, demographic mistakes, double-billing, and missing paperwork are some of the most common ones.
They make things more confusing, make people worry about money, and make people trust healthcare providers less.
Yes, doctors can resubmit corrected claims within payer deadlines.
They make sure rules are followed and things do not go wrong. This gives doctors more time to focus on their patients.
Doctors should perform internal billing audits at least quarterly.

