What is Revenue Cycle Management in Medical Billing?
- Author : Mark Twain
- Date : 26/10/2025
Every day, doctors care for patients and carry many responsibilities. Billing problems can harm a clinic’s future and patient trust. Revenue cycle management in medical billing helps convert care into correct payment.
RCM cycle in medical billing starts when a patient schedules an appointment and finishes with payment. It includes registration, coding, claims, payments, and denial handling. Doctors who learn RCM protect their income and reduce administrative stress.
This guide explains the process simply and with practical steps. You will learn tools, daily checks, and outsourcing options that help.
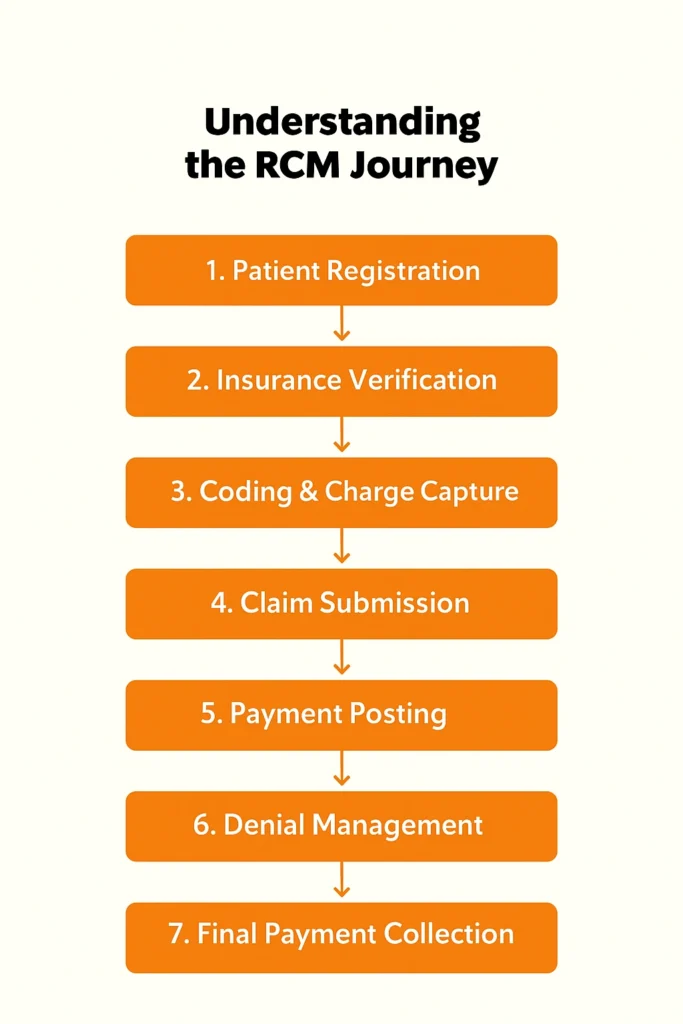
Understanding the RCM Journey
The RCM journey moves from patient intake to final payment collection. Every step must be accurate to avoid delays and denials. At pre-registration, collect full demographic and insurance details carefully. Verify patient eligibility and benefits before the visit starts.
During the visit, capture procedures and services clearly in the chart. Use correct CPT and ICD codes for each service provided. After service, submit clean claims to payers quickly and electronically.
Monitor adjudication and post payments as soon as they arrive. If a claim is denied, then identify the reason and correct documentation. Appeal quickly and track outcomes to prevent repeat denials.
A good medical billing revenue cycle keeps every step clean and fast. Clear workflows prevent delays and let doctors focus on patient care entirely.
Key Strategies Doctors Can Use Now
- First, fix front desk processes so that data is correct at intake. Many denials start with wrong or missing patient information.
- Second, add automation tools that validate code and check eligibility. Automation reduces manual errors and speeds claim submission.
- Third, set a denial team to appeal denials fast and track results. Quick appeals recover revenue before it is lost to time limits.
These are the trusted tips that the experienced billers at Mediclaim Pro Billing have been using successfully for years. We have added some fresh expert tips that our team recommends to help you get even better results.
Prevent Denials
Train the front desk team to collect all the necessary insurance and contact details from patients right from the start. Use digital forms that do not let anyone skip important fields, so the process is smoother and reduces errors.
Before beginning any treatment must take a moment to verify the patient’s coverage and see if prior authorization is required. Doing this early on can prevent a lot of claim denials and save you the hassle of dealing with time-consuming appeals later.
Use Automation
Link your EHR and billing systems so data moves automatically between them, no more repeating the same information or dealing with avoidable mistakes. Claim scrubbers are also a big help; they automatically check codes and payer rules to catch errors before claims go out.
Smart tools can even warn you about claims that might get denied, giving you a chance to fix them early. With automation handling most of the heavy lifting, your team can work faster or can reduce stress and keep the medical billing revenue cycle running smoothly.
When to Outsource Parts of RCM?
Consider outsourcing complex coding tasks or denial appeals to experienced billing partners, such as MediClaim Pro Billing, who know the job well. When you outsource, you not only save time but you also avoid making mistakes that could cause payments to be held up.
The right outsourcing partner can lower costs and give you access to experts who understand your specialty and local payer rules, and make your revenue cycle much more efficient. You can also monitor progress through dashboards and regular reports from your partners.
Manual vs Managed RCM - The Difference You Should Know
Factor | Manual RCM | Managed RCM |
Claim accuracy | Lower | Higher |
Time to payment | Longer | Faster |
Staff Workload | Heavy | Lower |
Revenue Growth | Slow | Steady |
- Manual RCM: You handle billing yourself (more control, more work).
- Managed RCM: Experts handle it for you (less stress, better efficiency).
How Technology Helps Modern RCM Tools
Software that checks eligibility and validates codes saves time. Cloud dashboards show claim status and accounts in real time. Modern tools reduce error rates and free staff for patient work. They can improve revenue cycle management in medical billing performance across your practice.
When your RCM process runs smoothly, your cash flow becomes steady and your income more predictable. That kind of financial stability lets you plan ahead with confidence, whether it is hiring more staff and buying new equipment or adding new services for your patients.
Patients also feel the difference. When bills are clear and there are no unexpected charges, they trust your practice more. Good billing habits do not just keep patients happy; they encourage them to come back and even recommend your services to others.
Pro Tips for Strong RCM in Healthcare
- Review denials within 48 hours to avoid losing appeal windows.
- Small tasks done once a week keep monthly backlogs and stress at bay.
- Use checklists at registration to prevent missing information.
- A short double-check saves hours of rework later.
- Track denial trends by payer to spot systemic issues quickly.
- Address root causes rather than repeating the same fixes.
Common Denial Reasons and Practical Fixes
Insurance mismatches and patient data errors are the top denials. Missing authorizations and medical necessity documentation also cause denials. For each denial, record the payer, code, and reason immediately. Use this data to fix processes and prevent repeats.
Applying a strong revenue cycle in medical billing reduces denials caused by data errors. Front-end checks and automated validation catch most simple mistakes.
A simple daily workflow keeps claims moving and avoids bottlenecks. Morning checks include eligibility, authorizations, and scheduled claims. Afternoon tasks focus on posting payments and reviewing denied claims. Daily small tasks prevent large end-of-month backlogs and stress.
KPI Details and How to Read Them
Understanding your key performance indicators is the first step to improving your billing process. Denial rate shows the percentage of claims rejected the first time they are submitted. This number keeps going up, which usually means that there are issues with registering patients and making mistakes with the code or not following the rules set by the payer correctly.
Days in A/R
The days in A/R metric tells you how long, on average, it takes to collect payments. When this number is high, it is a sign that money is getting stuck in the system, creating cash flow issues. Keeping your A/R days low helps your practice maintain steady income and financial stability.
Clean Claim Rate
Clean claim rate measures how many claims get accepted on the first try without any edits or resubmissions. The higher this rate the smoother your revenue cycle runs. Improving front-end accuracy and coding quality can help raise this number and speed up your overall revenue collection.
How to Choose an RCM Partner
Being able to trust the person handling your billing is very important when choosing an RCM partner. Find a team that has worked with clients like you before and has experience in your field. Reviewing sites or calling their references can help you figure it out. How trustworthy they are and how well they’ve done similar work in the past.
Before you decide, first ask a few questions. Find out how often their claims get denied or how successful they are with appeals, and how quickly they usually get payments processed. These numbers can give you a clear idea of whether they will actually make your billing more efficient.
Do not forget about data security. The company should follow HIPAA rules and safely handle patient information. Demand dashboards and weekly reports to stay informed and in charge even when work is being done from afar.
A Simple 90 Day Action Plan for Doctors
- Day 1 through Day 30: Fix the front desk checks and begin daily claim scrubs.
- Day 31 to 60: Add automation tools and train staff on common denials.
- Day 61 to 90: Review KPI trends and test outsourcing for appeals.
- After 90 days, keep checking in every week and doing checks every month.
Conclusion
In simple terms, RCM in healthcare covers everything from the moment a patient checks in to when the final payment is received. It is about keeping every step, like front-end checks, automation, denial management, KPI tracking, and staff training, running smoothly so nothing slips through the cracks.
When your RCM process works well, your revenue stays protected or your team stays focused, and your patients get better care. In the end, strong RCM is not just about collecting payments; it is about creating a healthier and more efficient practice that is built to grow.
Frequently Asked Questions
It is the whole journey of a medical bill starting when a patient registers and ending when the final payment comes in. It keeps everything organized so payments do not slip through the cracks.
RCM is like the work that goes on behind the scenes to keep the money flowing. It includes checking insurance as well as adding correct codes, sending claims and fixing any denials that come back.
RCM takes away the stress of paperwork. With smoother billing, doctors get paid faster and can spend more time actually caring for their patients.
A payer is the actual insurance company (e.g., Medicare, Aetna, Blue Cross) that reviews and reimburses claims based on the patient’s coverage.
Experts should sometimes be trusted with the tough jobs. Outsourcing speeds up the process or lowers costs. Look out for wrong billing, too, but do not put too much stress on your team.

