Internal Medicine Medical Billing: A Complete Guide for Healthcare Practices
- Author : Mark Twain
- Date : 26/10/2025
Internal medicine is one of the most diverse specialties in the healthcare department. It deals with complex diseases and lifelong chronic conditions. Internal medicine specialists (internists) often struggle to manage endless administrative and clinical tasks on a common day. These overwhelming responsibilities, especially billing, slow them down
The only rational solution is to have an internal medicine medical billing service that handles all your billing-related tasks on your behalf. They meticulously help you prepare documentation, coding, and know the payer-specific rules. These billing processes are too complex because internists handle a variety of conditions
In this blog, we will talk about internal medicine medical billing and the reasons to choose a billing service for your internal medicine practice. We will also see the ins and outs of the internal medicine practice. So let’s get into the details.
What Is Internal Medicine?
Internal medicine is a subfield and a medical specialty in the healthcare department that focuses on various diseases in adults. Internists are trained to diagnose and treat a broad spectrum of conditions, including multi-system diseases and common illnesses
They treat long-term comprehensive care conditions and chronic diseases like diabetes, hypertension, and thyroid problems. One of their main tasks is to coordinate with other general care providers for rendering help in specific internal medicine processes and diagnosis.
What is Internal Medicine Medical Billing?
Internal medicine medical billing refers to the process by which the diverse and complex services rendered by internists are converted into clean codes and claims. These codes are vital because they can make or break your revenue cycle. The billing process also needs to be precise because the internal medicine processes are sensitive, and even a minor error can cause claim denials or delays.
Internists also manage and handle various conditions simultaneously on a single visit because of the nature of their specialty. This multitasking translates to more documentation and coding layers to be dealt with. That is the sole reason why internal medicine is considered to be the most challenging specialty in terms of medical billing.
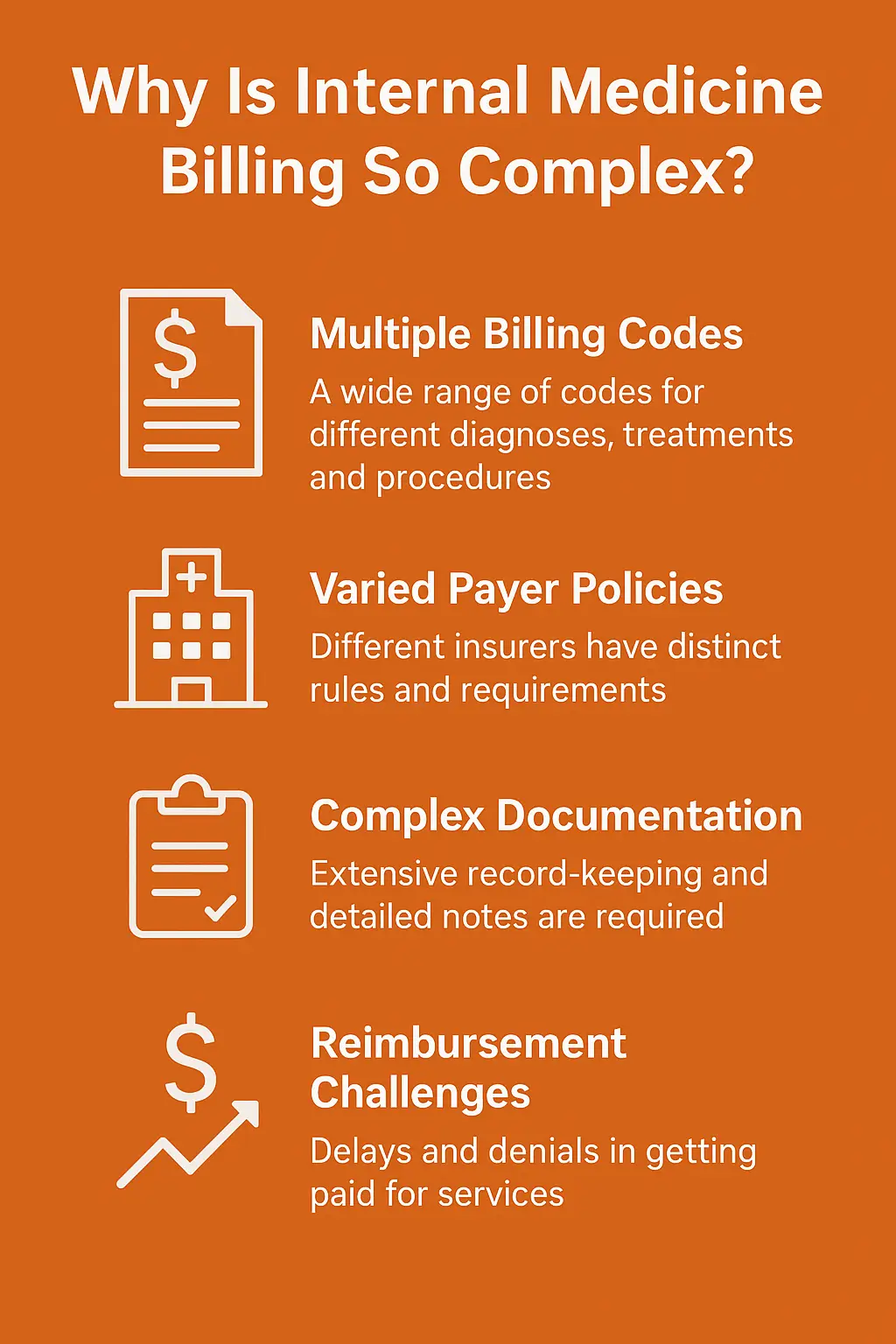
Why Is Internal Medicine Billing So Complex?
As we discussed earlier, there are various factors that make internal medicine medical billing complex. Some of them are mentioned here:
Range of Services
Internal medicine practices deal with a broad spectrum of services daily. These services include annual healthcare visits, chronic disease management, and complex diagnosis. All of these services fall under different codes that require concentration and extra care.
Similarly, many practices deal with cases that have more than one medical condition. It makes the billing process difficult. A patient with hypertension may also be struggling with diabetes and other conditions. That is why this billing process takes more time and effort than usual.
Multiple Chronic Conditions
Secondly, these internal medicine clinics handle multiple chronic conditions at a time. This multi-management approach not only includes continuous follow-ups, but also the diagnosis and care coordination. These conditions are usually time-sensitive, and they must be dealt with extreme care and concentration.
Additionally, preparing and submitting claims for different services and processes at the same time for the same individual is hectic. There are more chances that some errors seep through the cracks that ultimately damage the revenue stream.
Time-Based Billing Requirements
Internal medicine services depend largely on time documentation. It means you need to record and present time logs and proof of the work performed. Usually, these requirements are necessary for transitional care, advanced planning, and prolonged services. An unmatched time can lead to denial, even if the services are rendered legitimately.
Additionally, this type of billing also involves overlaps with decision-making. The choice of the method or time is critical because a wrong choice can damage your reimbursement. Time-based aspect is one of the most sensitive areas of internal medicine medical billing.
Frequent Code Updates
Keeping you and your medical knowledge up-to-date is critical, as even a small change can delay or cancel your reimbursement. Your codes need to be updated, and there must be no deleted or missing codes for a service provided.
Moreover, insurance providers usually have their own rules and regulations, and these regulations are changed annually. Knowing the updated regulations is crucial so that you may not get denials or late reimbursements for your services.
High Payer Scrutiny
Internal medicine processes often involve high-level codes like 99214. Since these codes are high-end and yield more reimbursements, they are scrutinized on a higher level as well. This higher scrutiny means that the payer may ask for additional details, documentation, and reasons.
Even small gaps in your documentation process can lead you to outright denials. Internists need to ensure that every code is accurate and is supported by appropriate and necessary documentation with justification. If you don’t have an expert billing support, you may fall in the trap unintentionally and may also lose your hard-earned money.
Common CPT Codes Used in Internal Medicine
Here are some of the most commonly used CPT codes in internal medicine. However, they are not the only ones that internists use:
| CPT Code(s) | Service Description |
|---|---|
| 99213 – 99215 | Established patient visits based on medical decision-making |
| 99202 – 99205 | New patient visits |
| 99490 | Chronic Care Management (CCM) |
| 99495 – 99496 | Transitional Care Management (TCM) after hospital discharge |
| 93000 | Electrocardiogram (ECG) with interpretation |
| 36415 | Blood sample collection (venipuncture) |
| 94640 | Nebulizer therapy |
| 99396 – 99397 | Preventive or annual visits for adults |
Benefits of Outsourcing Internal Medicine Medical Billing
Here are some of the potential benefits of hiring a medical biller for your internal medicine practice:
- It reduces administrative burden so physicians can focus more on patient care.
- It minimizes billing errors through expert coders. They are familiar with internal medicine complexities and processes.
- These services improve claim accuracy and speed up reimbursements.
- They lower operational costs by eliminating the need for in-house billing staff.
- They also enhance revenue cycle performance with simplified billing processes.
- These services ensure compliance with constantly changing healthcare and payer regulations.
- They provide access to advanced technology without spending extra money.
- They promote financial transparency with detailed and real-time reporting.
- Billing services also reduce claim denials through verification and coding precision.
- They offer scalability to practices so they can grow without interruptions.
Your internal medicine practice is struggling with revenue loss, right?

Conclusion
Internal medicine practices handle sensitive processes and conditions where accuracy and efficiency are a must. These practices deal with hypertension, diabetes, and conditions that are prolonged in nature. Sometimes, the same patient may require multiple diagnoses and treatments. These are not mere treatments, but they require enhanced billing processes and documentation that are hectic for physicians.
Medical billing services offer virtual medical billers to internal medicine practices. These billers are well-versed in the specialty, and they handle claims, denials, codes, and other particulars of the billing system with accuracy and precision. They also know the HIPAA and other regulations and keep your billing documents within those limits.
If your internal medicine medical billing system is not generating revenue or there are loopholes in your revenue cycle management, you can also hire a specialized medical biller. They can boost your revenue significantly by taking charge of all the billing-related tasks of your practice. This not only improves your cash management but also leaves you with more time to spend with your family and friends.
Frequently Asked Questions
Internal medicine medical billing is the process of translating the diverse services provided by internists into accurate codes for submission to insurance payers. These services may include chronic care, preventive care, diagnostics, and acute treatment.
Internal medicine deals with multiple chronic conditions, preventive care, and acute illnesses in a single visit. Each service has its own coding rules, time-based requirements, and documentation standards. They make the billing process more detailed and prone to errors.
Outsourcing transfers administrative billing tasks to experts who ensure accurate coding, faster claim processing, fewer denials, and compliance with payer regulations. This allows physicians to focus on patient care while improving financial efficiency.
Professional billing companies continuously monitor CPT/ICD-10 updates, payer-specific guidelines, and Medicare rules. Their teams are trained to apply these changes accurately to avoid claim denials.
Reputable billing services like Mediclaim Pro Billing follow strict HIPAA and data privacy regulations. They use secure platforms to protect patient information while handling claims and documentation.

